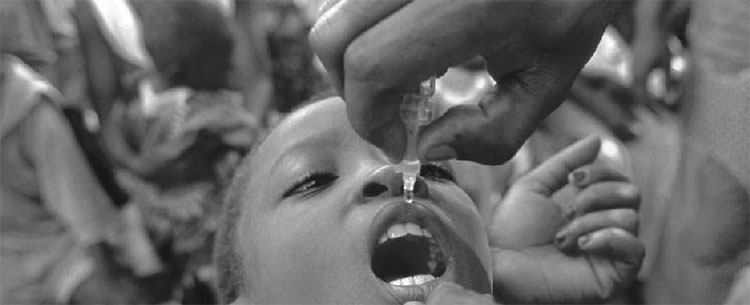
Ghana receives Global Fund 20th Anniversary Torch
The CCM Secretariat was host to the handing over ceremony of The Global Fund 20th Anniversary Torch. This kick starts the caravan activities starting from the 22nd of October to the 5th of November 2021.
There were speeches from:
- Program Manager, NACP
- NAP+ Ghana
- CCM Ghana
- UNAIDS Country Director
- GFAN Africa, and
- Global Fund
The closing remarks by Cecilia Senoo, Executive Director, Hope for Future Generations, and a Global Fund Board member, highlighted the activities to be carried out during the two (2) week period....